October Internal Assesment
4TH YEAR MBBS
We have been assigned to elog our internal assessment questions where the goal is to achieve learning driven through searchable information, particularly with regard to making original contributions and avoiding plagiarism from the searched work.
Here is my attempt of doing so.
Our question paper has been prepared as to assess our ability in our clinical postings regarding " Patient clinical data analysis" to develop our competancy in comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
NOTE: All the questions in the below question paper had been some of cases in our medical college in this past month.
QUESTION 1
DEFINE BONE DENSITY, HOW IS IT MEASURED? WHAT ARE THE CAUSES, CLINICAL FEATURES, DIAGNOSIS AND MANAGEMENT OF OSTEOPOROSIS?

Extra points taken from the below link
https://en.m.wikipedia.org/wiki/Osteoporosis
BONE DENSITY:
The amount of bone mineral in bone tissue is called bone density
MEASURING BONE DENSITY
- Z score: the number of standard deviations above or below the mean for the patient's age, sex and ethnicity.
- T score: the number of standard deviations above or below the mean for a healthy 30-year-old adult of the same sex and ethnicity as the patient.
OSTEOPOROSIS
Osteoporosis is defined as a bone density of 2.5 SD below that of a young adult.
Osteoporosis is a systemic skeletal disorder characterized by low bine mass, micro-architectural deterioration of bone tissue leading to bone fragility, and consequent increase in fracture risk.
Causes:
Osteoporosis may also occur due to a number of diseases or treatments, including alcoholism, anorexia, hyperthyroidism, kidney disease, and surgical removal of the ovaries. Certain medications increase the rate of bone loss, including some antiseizure medications, chemotherapy, proton pump inhibitors, selective serotonin reuptake inhibitors, and glucocorticosteroids. Smoking, and too little exercise are also risk factors.
Pathogenesis
The three main mechanisms by which osteoporosis develops are an inadequate peak bone mass (the skeleton develops insufficient mass and strength during growth), excessive bone resorption, and inadequate formation of new bone during remodeling, likely due to mesenchymal stem cells biasing away from the osteoblast and toward the marrow adipocyte lineage.
Diagnosis
Bio markers :Chemical biomarkers are a useful tool in detecting bone degradation. The enzyme cathepsin K breaks down type-I collagen, an important constituent in bones. Prepared antibodies can recognize the resulting fragment, called a neoepitope, as a way to diagnose osteoporosis. Increased urinary excretion of C-telopeptides, a type-I collagen breakdown product, also serves as a biomarker for osteoporosis.
2)DEFINE MYXOEDEMA COMA? DESCRIBE ITS CLINICAL FEATURES, DIAGNOSIS AND TREATMENT.
Extra points taken from the below link
https://en.m.wikipedia.org/wiki/Myxedema_coma
A person may have laboratory values identical to a "normal" hypothyroid state, but a stressful event (such as an infection, myocardial infarction, or stroke) precipitates the myxedema coma state, usually in the elderly.
Clinical feature
- Cardiovascular
- Bradycardia
- Bundle branch blocks
- Complete heart block and arrhythmias
- Cardiomegaly
- Elevated diastolic blood pressure—early
- Hypotension—late
- Low cardiac output
- Non-specific ECG findings
- Pericardial effusion
- Polymorphic ventricular tachycardia (torsades de pointes)
- Prolonged QT interval
- Respiratory
- Hypoxia
- Hypercarbia
- Hyperventilation
- Myxedema of the larynx
- Pleural effusion
- Gastrointestinal
- Abdominal distention
- Abdominal pain
- Anasarca
- Anorexia and nausea
- Decreased motility
- Fecal impaction and constipation
- Gastric Atony
- Myxedema or toxic megacolon—late
- Neurogenic oropharyngeal dysphagia
- Paralytic ileus
- Neurological
- Altered mentation
- Coma
- Confusion and obtundation
- Delayed tendon reflexes
- Depression
- Poor cognitive function
- Psychosis
- Seizures
- Renal and urinary function
- Bladder dystonia and distension
- Fluid retention
- Appearance and dermatological
- Alopecia
- Coarse, sparse hair
- Dry, cool, doughy skin
- Myxedematous face
- Generalized swelling
- Goiter
- Macroglossia
- Non-pitting edema
- Ptosis
- Periorbital edema
- Surgical scar from prior thyroidectomy
- Hypothermia
Laboratory features in myxedema coma:[
- Anemia
- Elevated creatine kinase (CPK)
- Elevated creatinine
- Elevated transaminases
- Hypercapnia
- Hypercholesterolemia (elevated LDL)
- Hyperlipidemia
- Hypoglycemia
- Hyponatremia
- Hypoxia
It extends from Cranial border of atlas to L1 vertebrae( lower border)
It’s caudal end consists of Conus medullaris which contains S3 S4 S5
SPINAL CORD LEAION LOCALISATION
AT THE LEVEL
Motor- Segmental LMN finding
Sensory- Segmental sensory root findings
BELOW THE LEVEL
Motor - UMN finding
Sensory- Tract involvement findings
Automatic- Bladder and Bowel findings
INTRA MEDULLARY LESION
Dysesthesia, Paresthesia
Dissociated sensory loss
Sacral spacing is present
Spastic paralysis not prominent
Muscle atrophy common
Tropic skin changes common
Bladder and bowel disturbances occur early if lesion is lower
EXTRAMEDULLARY LOCALISATION
Root pain
Segmental wasting
Spastic paralysis
Bladder and bowel symptoms occur late
LOCALISATION AT CONUS
Bladder incontinence
Bowel incontinence
Loss of penile Tunescence
Loss of anal reflex
Loss of Bulbocavernous reflex
Perinatal sensory loss
No motor weakness
5) CAUSES, DIAGNOSIS AND TREATMENT OF AYRIAL FIBRILLATION?
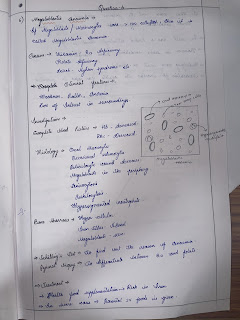
Megaloblastic anemia is a type of macrocytic anemia. An anemia is a red blood cell defect that can lead to an undersupply of oxygen. Megaloblastic anemia results from inhibition of DNA synthesis during red blood cell production. When DNA synthesis is impaired, the cell cycle cannot progress from the G2 growth stage to the mitosis (M) stage. This leads to continuing cell growth without division, which presents as macrocytosis
Ascites exists in three grades:
Grade 1: mild, only visible on ultrasound and CT
Grade 2: detectable with flank bulging and shifting dullness
Grade 3: directly visible, confirmed with the fluid wave/thrill test
Indications of dialysis in acute renal failure (ARF)
- Severe fluid overload
- Refractory hypertension
- Uncontrollable hyperkalemia
- Nausea, vomiting, poor appetite, gastritis with hemorrhage
- Lethargy, malaise, somnolence, stupor, coma, delirium, asterixis, tremor, seizures,
- Pericarditis (risk of hemorrhage or tamponade)
- bleeding diathesis (epistaxis, gastrointestinal (GI) bleeding and etc.)
- Severe metabolic acidosis
- Blood urea nitrogen (BUN) > 70–100 mg/dl
Indications of dialysis in chronic renal failure (CRF)
- Pericarditis
- Fluid overload or pulmonary edema refractory to diuretics
- Accelerated hypertension poorly responsive to antihypertensives
- Progressive uremic encephalopathy or neuropathy such as confusion, asterixis, myoclonus, wrist or foot drop, seizures
- Bleeding diathesis attributable to uremia






















Comments
Post a Comment