Injury to the right foot+DM+Hypertension+SOB
JAHNAVI CHATLA
MBBS 4th year
BLOG FOR PRACTICALS
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
This case is about a 65 year old Gentleman who was an RTC driver 15 years back
Although the patient has been changing hospitals since the past 30 days, I would like to start his history from 10 years back
10 YEARS AGO
The patient then was a 55 year old man working on different part time jobs for his Daily living
Driving rental cars
Works in his very own vegetable shop
He felt weak and not well for a few days for which he visited local hospital and was diagnosed to be Hypertensive
He was kept to Antihypertensives and now is on
T-Aten-Am 50mg
5 YEARS AGO
The patient one day was helping someone who was cutting a tree by holding the branch which was being cut with the help of a rope
He got injured by a stone in the rope to his left palm
This was followed by pain, swelling and blackish discolouration
Then was when he was diagonosed incidentally as diabetic and was kept on medication
He is now on Tab. Metformin 500mg
4 YEARS AGO
He drank and drove following which he had an accident
He drove back home and was taken to hospital from there.
There was
1.fracture to his Left ribs (5,6,7) at mid clavicular line
2.Punctured his lung when led to hemoptysis and suffered for a month
30 DAYS BACK
While he was going out for work, he stepped over a sharp stone which penetrated through his right little toe
He used medications from the local medical store for about 10 days
He noticed
1. Increase in pain gradual
2. Edema till his knee which was gradual
3. Bleb formation of about 3*3 cm on the dorsum of his foot which he ruptured by piercing a safety pin through it
There was bleeding from the site after piercing and it continued for a few days and formed into an ulcer.
4. Low grade on and off fever
5. There was difficulty in urination
Dysuria
Burning micturition
Hematuria
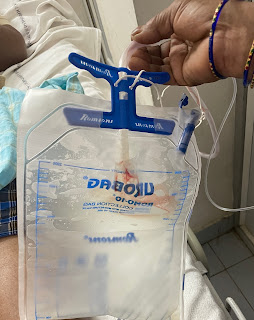
Reduced urine output
He then went to a government hospital in Nalgonda and was diagnosed to be AKI on CKD and was transferred for private hospital 1 for dialysis
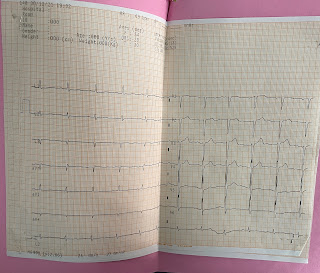
There he developed SOB of grade 2-3, orthopnea and PND
He unwent through Dialysis 1
Due to money restraint the patient was shifted to private hospital-2 9 days back
PRESENTATION
Ulcer of right foot since 20 days
Decreased urine output (dysuria, hematuria, burning micturition ) since 20 days
SOB of grade 2-3, orthopnea, PND since 10 days
Generalised anasarca
DAILYSIS 2
He had itching at his abdomen, back and left and right Axilla
DIALYSIS 3 and 4 done
Patient is feeling better comparatively but still has low urine output and SOB
PAST HISTORY
Alcoholic 90ml everyday since 40 years
Chronic smoker 1 pack since 40 years
Hypertensive since 10 years
Diabetic since 5 years
Not a case of Asthma, tuberculosis, epilepsy
FAMILY HISTORY
The patients mother is diabetic
None of the other family members have similar complaints
DRUG HISTORY
T-Aten-am 50mg
Metformin500mg
No known allergies
PERSONAL HISTORY
Diet- mixed
Appetite- reduced since 3 days
Sleep - inadequate
Bladder - decreased
Bowel- regular
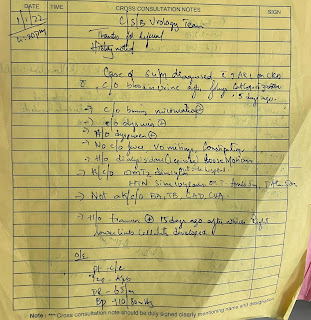
CROSS CONSULTATION NOTES
30/12/2021
GENERAL EXAMINATION
The patient is coherent conscious cooperative, and well oriented to time place and person
He is moderately built and nourished
Pallor- absent
Icterus- absent
Cyanosis- absent
Clubbing-absent
Edema- present pitting Type
Lymphedenopathy - absent
Vitals:

































Comments
Post a Comment