Prefinals 2
JAHNAVI CHATLA
MBBS 4
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
50 year old male patient, toddy collector by occupation, Alcoholic since 15 years (90 ml of whiskey) and chronic smoker since 25 years(20 beedi/day), resident of Yadhadhri has come to the op with the chief complaints of
1) Cough since 3 months
2) Fever since 1 month
3) Vomitings since 5 days
4) Giddiness since 5 days
7 YEARS AGO
The patient weighing around 50 kg,was apparently asymptomatic 7 years ago
Then he had episodes of vomitings.He was taken to hospital where he was found out to be having Right sided pneumonia. He was prescribed some medications and advised to stop alcohol and smoking.
He took the medication for about 1 month strictly and he stopped alcohol and smoking for that course of time.
He got back to his addictions after 1 month.
The patient got back to his regular activities after 1 month
3 YEARS AGO
He stopped collecting toddy as his children and wife found out that he was consuming more amount of it.
3 MONTHS AGO
Wet cough with sputum which was 2-3 spoons full, yellowish, foul smelling without blood tinge.
Sputum is more in the morning and cough is more at night. He used to wake up from his sleep
No medications were taken then
1 MONTH AGO
Fever which is insidious in onset, gradual in progression with no diurnal variation relieves on taking medications.
Diagnosed to be having Typhoid. Medications were prescribed but of no use.
The patient was weighing 35 kg around this time
22-3-2022
At night,The patient was unable to go to washroom on his own so asked for the help of his children
He felt giddy and became unconscious
ORS was given and patient was asked to sleep
After 1 hour, he had 2 episodes of vomiting which was non bilious, non foul smelling contained the ORS.
23-3-2022
He was to Hospital-1 where he had involuntary micturition and fell unconscious
The attendants have informed that his BP was low and was given fluids.
He was referred to Hospital 2 following which tests were done and diagnosed to be having Active Tuberculosis.
Present complaints
Cough since 3 years
Fever since 1 month
Giddiness since 5 days
27-3-2022
Patient had four episodes of loose motions
PAST HISTORY
Not a known case of DM HTN Asthama epilepsy
Didn’t receive any blood transfusions or underwent major surgeries
FAMILY HISTORY
Not significant
PERSONAL HISTORY
DIET- mixed
APETITE- decreased since 10 days
BLADDER MOVEMENTS - increased
BOWEL MOVEMENTS- Regular
SLEEP- adequate
ALLERGIES - none
GENERAL EXAMINATION
The patient is conscious coherent and cooperative, well oriented to time place and person
He is poorly built and nourished weighing 40 kg
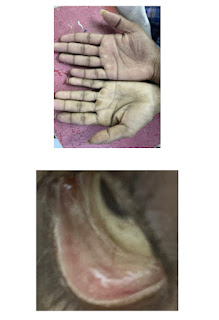
Pallor- present
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Edema -absent
VITALS
27-3-2022 vitals
Temp- 99.6
Pulse rate- 81bpm
Rr- 16cpm
BP -110/70 mmhg
SYSTEMIC EXAMINATION
CVS- S1 S2 heard. No other murmurs heard
CNS- Higher motor functions intact
GIT- Abdomen is soft non tender and scaphoid
No features of hepatosplenomegaly
RESPIRATORY EXAMINATION
INSPECTION
Shape- Flattened
Accessory respiratory muscle movements- absent
Trial’s sign- negative
Trachea- appears to be central
Apex beat- appears to be near the 5th inter coastal space
Supraclavicular hollow- present
Infraclavicular flattening - present
Suprascapular wasting - present
Shoulder drooping - absent
Scoliosis/kyphosis/lordosis- absent
No engorged vein sinus or scars seen
PALPATION
All inspectatory findings have been confirmed
There is no rise of local temperature or tenderness
Trachea- central
Chest movements- Reduced on the right side
Vocal fremitus-reduced on the right side
Rib crowding - absent
Bong tenderness- absent
Measurements
Ap- 6 inches
Transverse -10.5 inches
PERCUSSION
Right side dull note at mammary and inframammary areas
Left side resonant
AUSCULTATION
Right side - breath sounds reduced
Left side - normal
No rhonchi or wheeze heard
INVESTIGATIONS
CBP
RBS 146
Hba1c 6.5
Hb 7.58
TLC 9500
Neutrophils 90
Lymphocytes 4
Monocytes 3
Esinophils 3
Platlets 2.51lakhs
LFT
Total bilirubin 2.83
Direct bilirubin 1.25
AST 230
ALT 175
A/G 1.16
ALP 230
Total proteins 4.2
Albumin 2.26
SERUM ELECTROLYTES
EF-55%
Trivial Tr+/no Mr , trivial Ar+
Good LV systolic function +
Diastolic dysfunction +
USG abdomen :
Findings: 1)E/O air bronchogarm in right lung
2)E/O 5 mm hyperechoic focus noted adherent to Gb wall
Imp:
1) Gall bladder wall edema
2) right lung consolidation
3)gall bladder wall polyp
X-RayDIAGNOSIS
HYPOKALEMIC PERIODIC PARALYSIS SECONDARY TO ? ACUTE GE ?ALCOHOL
WITH RIGHT LOWER LOBE PNEUMONIA
WITH ALCOHOLIC HEPATITIS
WITH DYSELECTROLYTEMIA
1) Ivf ns/ rl @ 100 ml/hr
2)Inj pantop 40 mg IV/od
3)Inj zoefer 4 mg IV/sos
4)tab udilin 500mg po/BD
5)syp potlhlor 10 ml po/tid in glass of water
6)INJ monocef 1gm/IV/BD (day1)
7)2 scoop of protein powder in 100 ml milk/ water po/TID
8)Ascoryl syrup po/TID
9)monitor vitals hourly





















Comments
Post a Comment